Reliable routine health system data — at last? The added value of an integrated DHIS2 and RBF data system
A large number of countries in which we work have shifted their HMIS (health management information system) onto DHIS2 — a popular open source software tool developed by the University of Oslo. Often, the data platform also becomes the country’s de-facto health system data warehouse.
While using DHIS2 has many clear advantages, one major benefit for countries is that it allows for the integration of multiple vertical data systems into a single data platform. In other words, data collected through one system becomes available to all through a centralized hub. For example, HIV, TB (tuberculosis), NCD (non-communicable disease) specific data systems can now be merged into the national DHIS2.
However, DHIS2 does not solve the issue of data reliability. Meaning that the technology alone cannot solve issues related to the poor quality of reported data, irregular reporting and perverse incentives. But results-based-financing (RBF) can.
RBF adds value to routine data systems in three concrete ways:
- RBF creates an incentive for better management of data at both health care facility and district levels. Why? Because once money is tied to data, stakeholders tend to care more about data. Linking health facility financing to data leads to better data completeness and reporting.
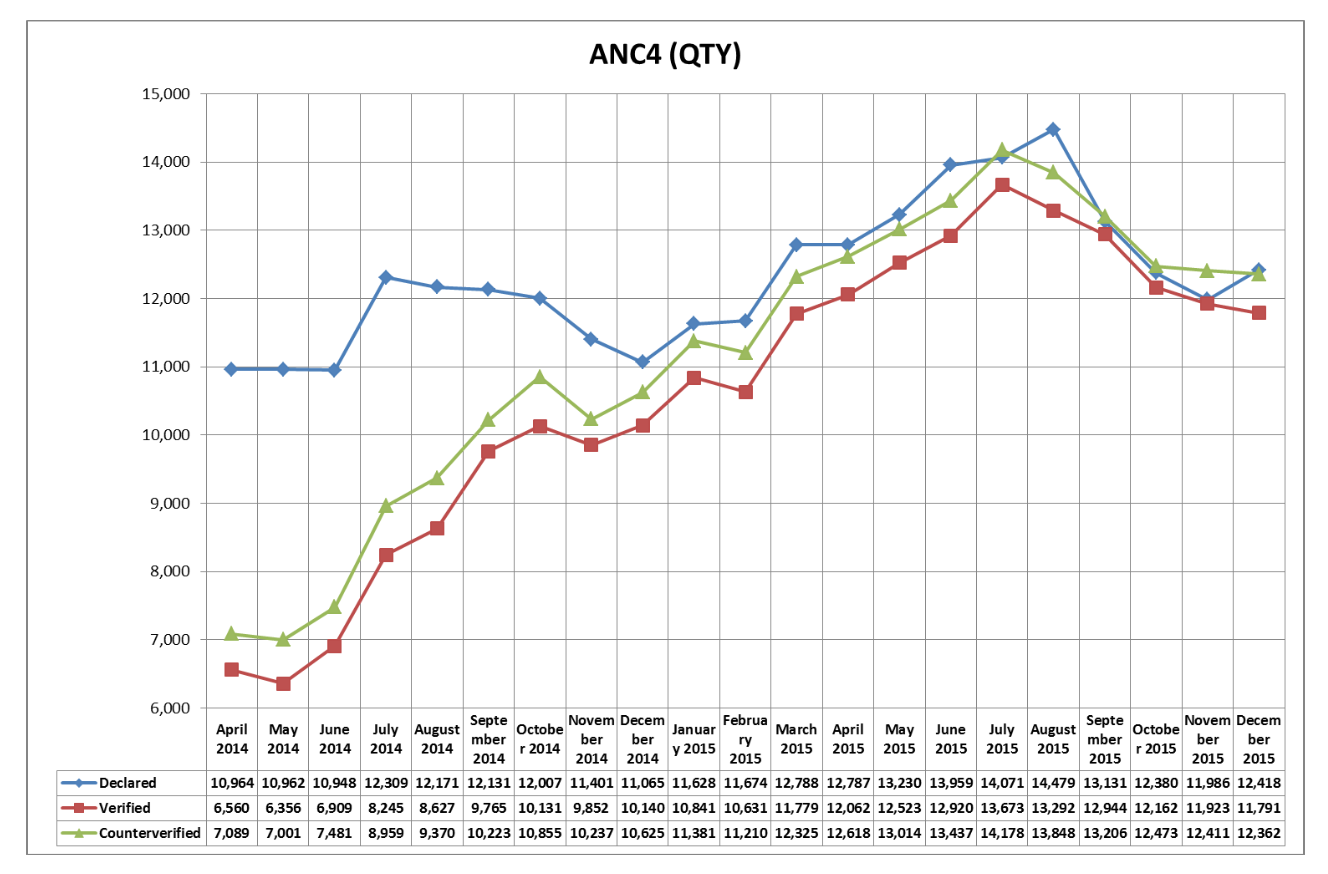
- Data verification mechanisms have been developed in most countries using RBF systems. External teams visit a given facility on a regular basis and triangulate the declared data to check its accuracy. In several countries, the difference between declared data and verified data has gradually been reduced over time, showing an overall improvement on how health care facilities manage and report data.
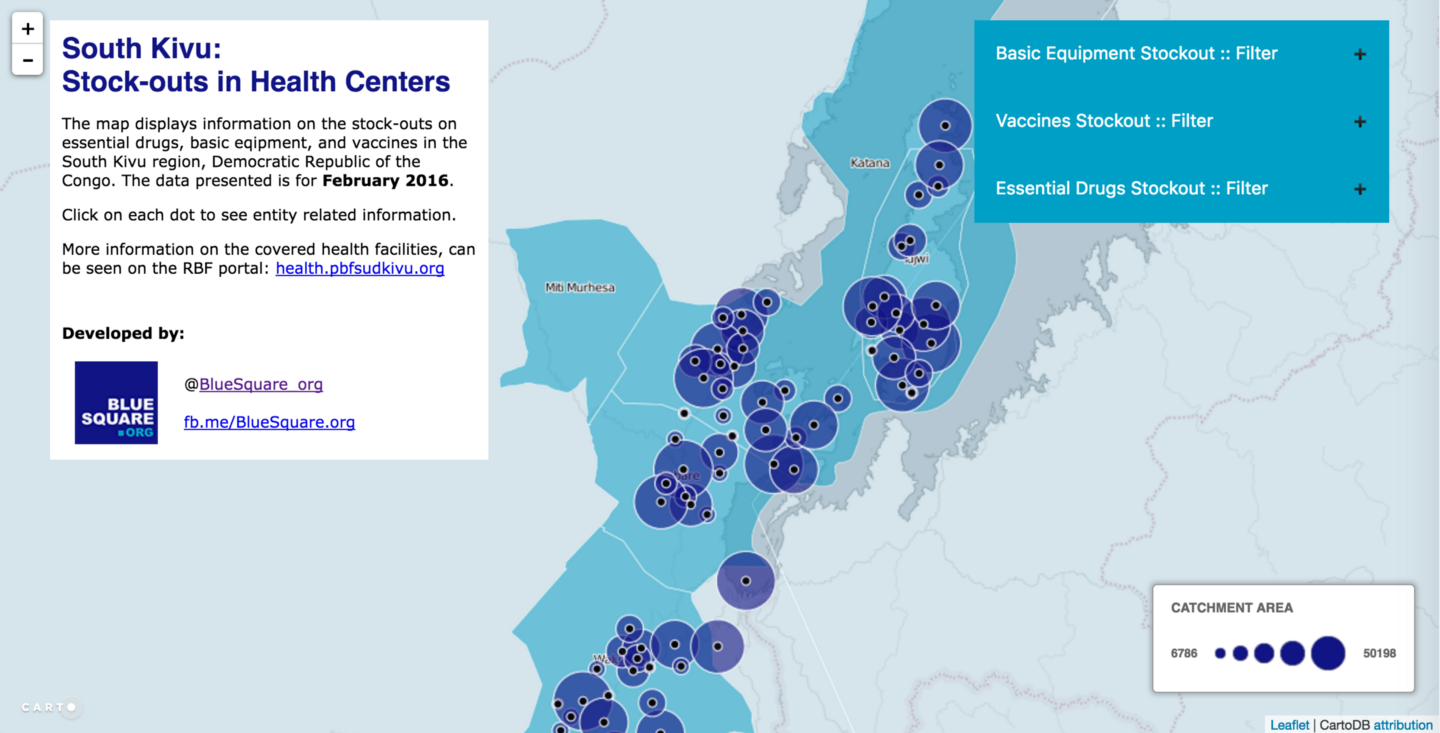
- Finally, in most countries that implement RBF routine, quality of care evaluations are being conducted, often on a quarterly basis. To do this, a structural quality checklist is frequently used as a proxy for quality of care measurement. These checklists focus on service availability and readiness, and are a simpler version of the typical SARA questionnaire. BlueSquare currently helps seven countries digitize this structural quality measurement evaluation. In shifting these routine health care surveys carried out as part of RBF on mobile devices, countries can start to collect 100–200 data elements per health care facility per quarter. In that sense, RBF brings a new “externally verified service availability and readiness” data set to routine HMIS systems.
To recap, the integration of RBF and DHIS2 platforms is of high value to HMIS data. It brings better, verified data, and a new large routine service availability and readiness data set.
As a result, several countries, including Benin, Democratic Republic of Congo, and Kenya are asking us to connect and integrate RBF and DHIS2 platforms. This interoperability requires an alignment of the health system hierarchy (the org unit hierarchy in DHIS2) and an alignment of the RBF “indicators” with the DHIS2 “data elements”.
Once this is in place, interoperability has several advantages:
First, declared data from health care providers is collected only once through the HMIS. Secondly, the national DHIS2 platform is used for RBF monitoring and evaluation (M&E). Third, any “RBF” data (verified, quality of care, patient feedback) is available for any other program in the DHIS2 platform.

But, the biggest advantage is yet to come. By bringing HMIS and RBF data together, countries will be able to: combine routine verified output data for coverage measurement with routine service availability and readiness data in a way that will help constantly monitor primary health care vital signs in a totally new way.
Written by Nicolas de Borman, Founder & CEO of BlueSquare. Find him on LinkedIn here and Twitter here.