July 1st, 2025
Campaign digitalization Georegistry
Digitalisation of the Health Facility Registry – A Comprehensive Suite Offered by Bluesquare
Over the past few years, Bluesquare has specialised in managing digital health facility registries. Role and Purpose of Digital Health Facility Registries Digital health facility registries play […]

March 24th, 2025
Global health RMNCAH & Nutrition
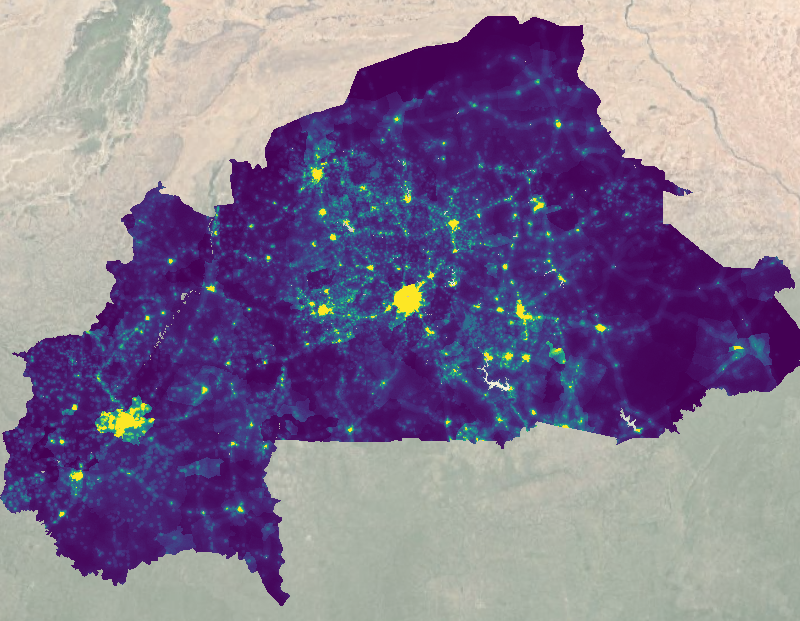
A Data-Driven Platform Supporting Pastoralism in the Sahel Region
Since 2023, PRAPS-2, with the technical support of Bluesquare, has developed an innovative monitoring and evaluation platform to support pastoralism in the Sahel. Bluesquare was recruited by […]

March 4th, 2025
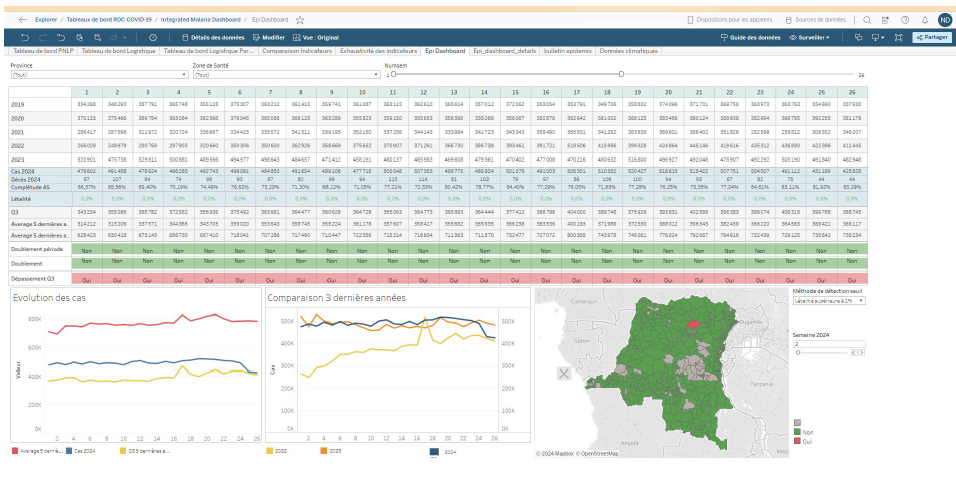
Campaign digitalization Epidemic prone diseases surveillance Global health Malaria, HIV, TB
5 Myths About Health Campaign Digitalization
Digitizing health campaigns: Debunking common misconceptions! Is digitalizing health campaigns too expensive? Too complex? Too risky? Many health organizations hesitate to embrace digital solutions for health campaigns […]

October 1st, 2024
Campaign digitalization Events & webinars Georegistry Global health Malaria, HIV, TB
Bluesquare at Geopalooza 4.0: A look at the latest in geospatial innovation
Bluesquare participated at Geopalooza 4.0 from July 22 to 26, 2024 in Nairobi, Kenya where the team highlighted innovative approaches to use routine activity field data for […]
Load more
Most read
These posts have brought some attention

December 28th, 2018
Epidemic prone diseases surveillance Projects
The Trypelim project: digital tools to help eliminate Sleeping Sickness
Sleeping Sickness is a parasitic disease transmitted by the tsetse fly. It is lethal in most cases. The disease has been an important cause of death in […]

June 12th, 2021
Epidemic prone diseases surveillance Global health Malaria, HIV, TB Press Projects
L’Echo: Bluesquare, the (not so) small Belgian who seduces the Bill & Melinda Gates Foundation
Original article written by Simon Souris for L’Echo. Inefficiencies in the development aid funding chain have damaging consequences: every year, several billion euros collected from private donors […]

March 17th, 2022
Health financing Projects
Increasing health insurance access in LMICs: the ambition of openIMIS
This case study was part of our 2022 Impact Report. Digitizing health insurance management processes is key when it comes to the quality development and accessibility of […]

October 1st, 2024
Campaign digitalization Events & webinars Georegistry Global health Malaria, HIV, TB
Bluesquare at Geopalooza 4.0: A look at the latest in geospatial innovation
Bluesquare participated at Geopalooza 4.0 from July 22 to 26, 2024 in Nairobi, Kenya where the team highlighted innovative approaches to use routine activity field data for […]